Improved Heart Failure Outcomes Begin with Updated Order Sets
Heart failure’s cost runs deep for patients, families and Canada’s healthcare system.
Does your team have up-to-date, evidence-based clinical standards in place to drive optimal outcomes for your patients?
Heart Failure in Canada
Over 650,000 Canadians 40 years of age and older live with a heart failure diagnosis.1
Each year, over 92,000 Canadians receive a new heart failure diagnosis.2
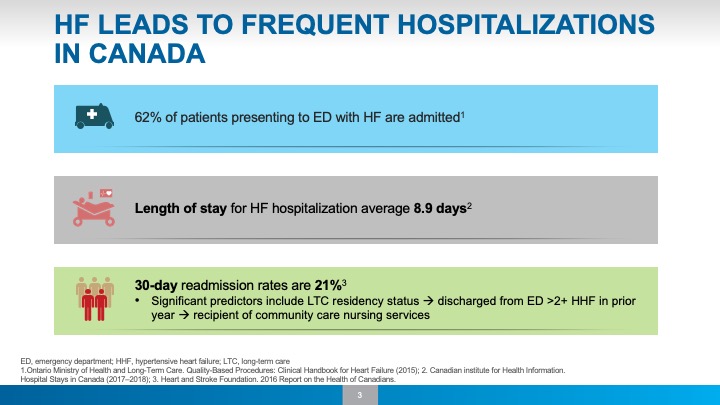
For someone 65 and older, heart failure is the second most likely reason they’ll be hospitalized (heart attacks rank third).3
On average, a heart failure admission lasts 8.9 days and costs our healthcare system $10,970 per visit.4
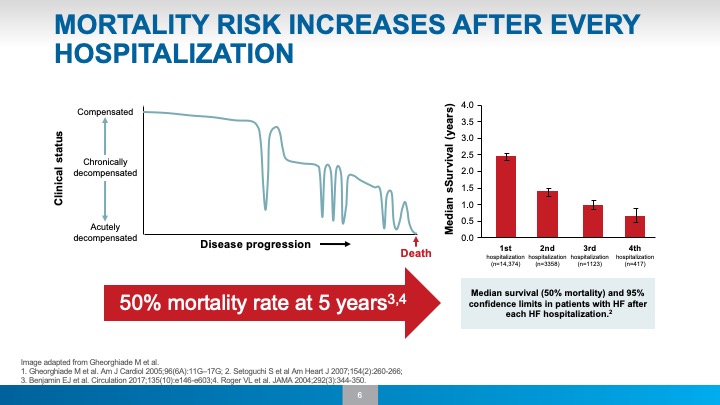
The Risk of Repeat Heart Failure Hospitalizations
Heart failure is a progressive disease. Mortality rates are high.
With each hospitalization, the risk of readmission rises and life expectancy decreases. Within 30 days of discharge, 21% of heart failure patients are readmitted for follow-up care.5


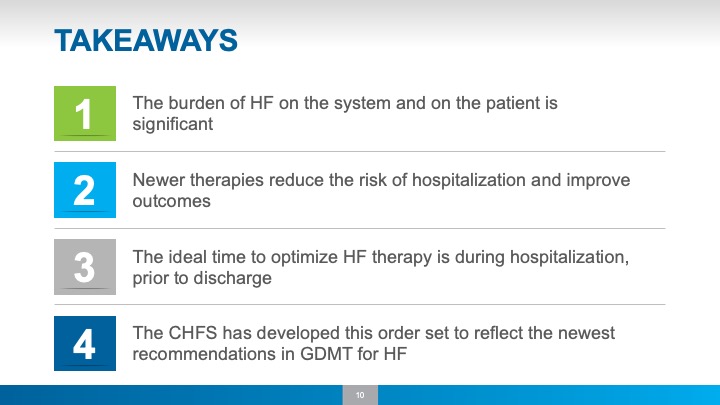
Heart failure burdens Canadian families and our health system. Now more than ever, we have new research, tools and devices to treat and prevent heart failure.
When structured into better tools and processes, this new knowledge can make a difference in treating heart failure and preventing hospital readmissions. But only if it makes it to the patient.
The Canadian Heart Failure Society (CHFS) has updated their standard heart failure Order Sets to align with up-to-date, evidence-based research.
Average Number of Out-Of-Hospital Days is Reduced by 28 in Between Each Rehospitalization
Each time patients are admitted, they are back in the hospital 1 month faster than the last time.
Hospital Admissions: A Key Stage to Improve Heart Failure Outcomes
“There’s often a tendency to just say, ‘Let’s wait until we see the patient back in the clinic in a couple of weeks after hospital discharge.’ But the reality is that so often things are incredibly busy in the outpatient setting and many patients never get started on the right medications if we delay. Our message is to act now and help patients get the greatest benefits as early as possible.”
Dr. Robert Mentz, lead investigator of PRIME-HF7
Pathway To Improve Heart Failure Outcomes Begins At Admission
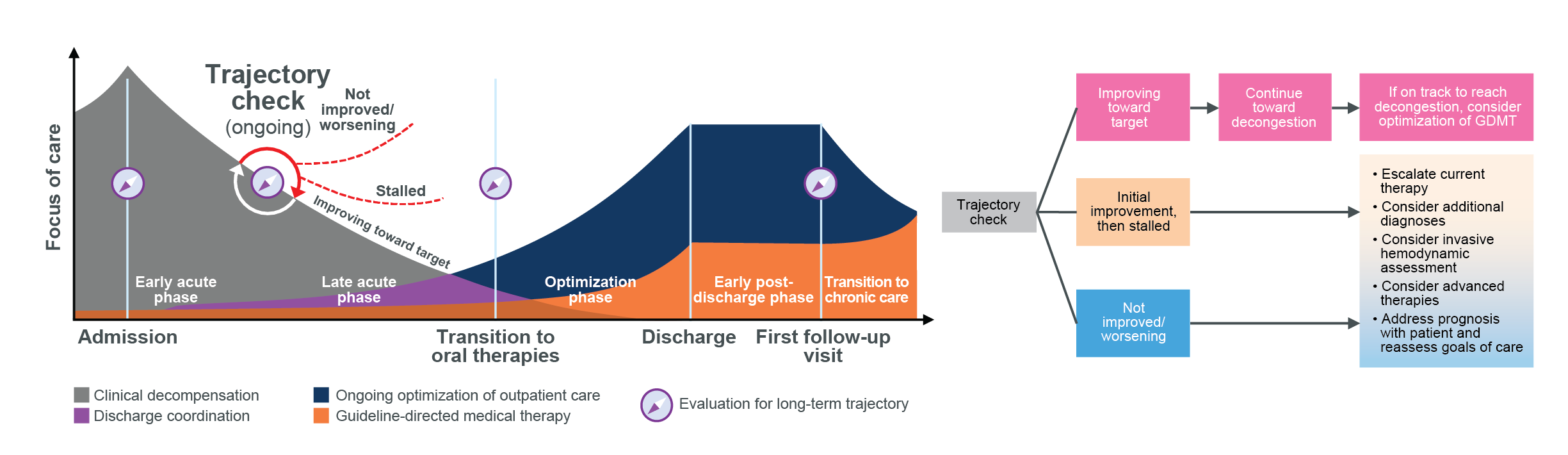
In this audio clip, Dr. Shelley Zieroth, Past President of the Canadian Heart Failure Society, describes how discharge coordination, an ongoing coordinated focus on outpatient care, and optimized, guideline-directed medical therapy can change the long-term trajectory for a patient’s heart failure journey.
Admissions are a critical stage in treating heart failure, and provide a unique opportunity to improve care for patients with this condition.
Discharge Planning
Strategies to reduce readmission rates include early patient discharge planning and scheduling follow-up appointments prior to discharge.
Patients should be provided with self-care tools before discharge. Detecting subtle changes in symptoms early is a key skill for heart failure patients to develop and integrate in their daily lives.
Daily diary use is a proven method to keep track of symptoms and recognize early signs of decompensation. Greater diary use is associated with better heart failure outcomes and longer survival rates.
CHFS has collaborated with patients to develop a Patient Diary to accompany them on their journey. We encourage healthcare professionals to download the document and provide it to their patients at discharge

Overcoming Inertia
Download the updated CHFS Order Set
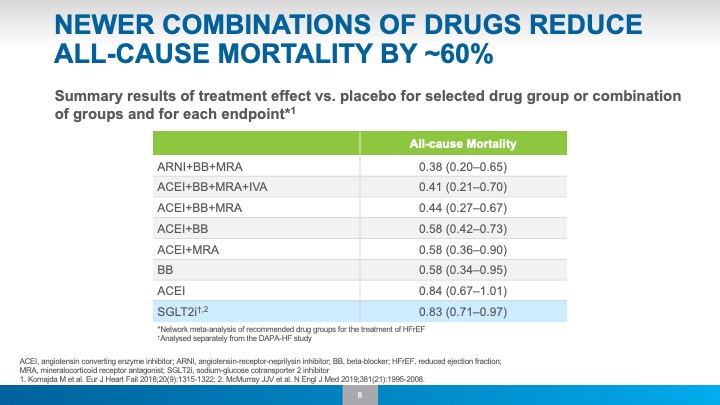
Clinical trials involving guideline-directed medical therapies (GDMT) have been shown to improve patient outcomes and reduce costs to healthcare systems.
Inertia, however, is a known barrier to instituting evidence-based therapies. Clinicians and health systems have many priorities and commitments. The time required to update documentation and train clinical staff can easily become the positive intention that is months or years delayed.
The new CHFS order set is designed to make it easy to keep your clinical protocols in line with the latest evidence-based recommendations.

2021 CHFS Heart Failure Admission Order Set Update
Join us for a live webinar on the new 2021 CHFS Heart Failure Admission Order Set
About CHFS
The Canadian Heart Failure Society’s (CHFS) mission is to improve patient care through research, advocacy, education and the development of best practices in the field of heart failure disorders.
CHFS Order Set Executive Committee

- Dr. Anique Ducharme -
MD, MSc, FRCP
Professor of Medicine, Université de Montréal
Director, Heart Failure Clinic
Montreal Heart Institute, Research Center
President, Canadian Heart Failure Society
Montreal, QC

- Dr. Jonathan Howlett -
MD, FRCPC, FCCS, FHFSA(Hon)
Clinical Professor of Medicine, University of Calgary
Libin Cardiovascular Institute of Alberta, South Health Campus, Calgary
Past & Founding President, Canadian Heart Failure Society
Calgary, AB

- Dr. Shelley Zieroth -
MD, FRCPC, FCCS, FHFSA, FESC, FACC
Professor, Cardiology, University of Manitoba
Director, SBH HF and Transplant Clinics
Head, Medical HF Program, WRHA Cardiac Sciences
Past President, Canadian Heart Failure Society
Winnipeg, MB

- Dr. Stephanie Poon -
MD, MSc, FRCPC
Medical Director, Heart Function Clinic
Cardiologist, Sunnybrook Health Sciences Centre
Assistant Professor, University of Toronto
Toronto, ON
Contact Us
Canadian Heart Failure Society (CHFS)
1100-222 Queen Street
Ottawa, ON K1P 5V9
Tel: 1.877.569.3407, ext.418
@CanHFSociety
Visit us online at https://heartfailure.ca/
Footnotes
1, 2) 2017 Heart disease in Canada: Highlights from the Canadian Chronic Disease Surveillance System.
3) A snapshot of Health in Canada as Demonstrated by Top 10 Lists. Canadian institute for Health Information. Hospital Stays in Canada (2017–18).
4) Canadian institute for Health Information. Hospital Stays in Canada (2017–18).
5) O’Connor, Christopher M. “High Heart Failure Readmission Rates: Is it the Health System’s Fault?” JACC: Heart Failure, May 2017
6) Bakal, Jeffrey A., et al. “Heart Failure Re-Admission: Measuring the Ever Shortening Gap between Repeat Heart Failure Hospitalizations.” PLoS ONE, vol. 9, no. 9, 2014, doi:10.1371/journal.pone.0106494.
7) Ivabradine use more consistent in HF patients with in-hospital recommendation
This content was exclusively developed by the Canadian Heart Failure Society, a not-for-profit medical society that receives support from commercial partners to support their educational activities. For more information click here.